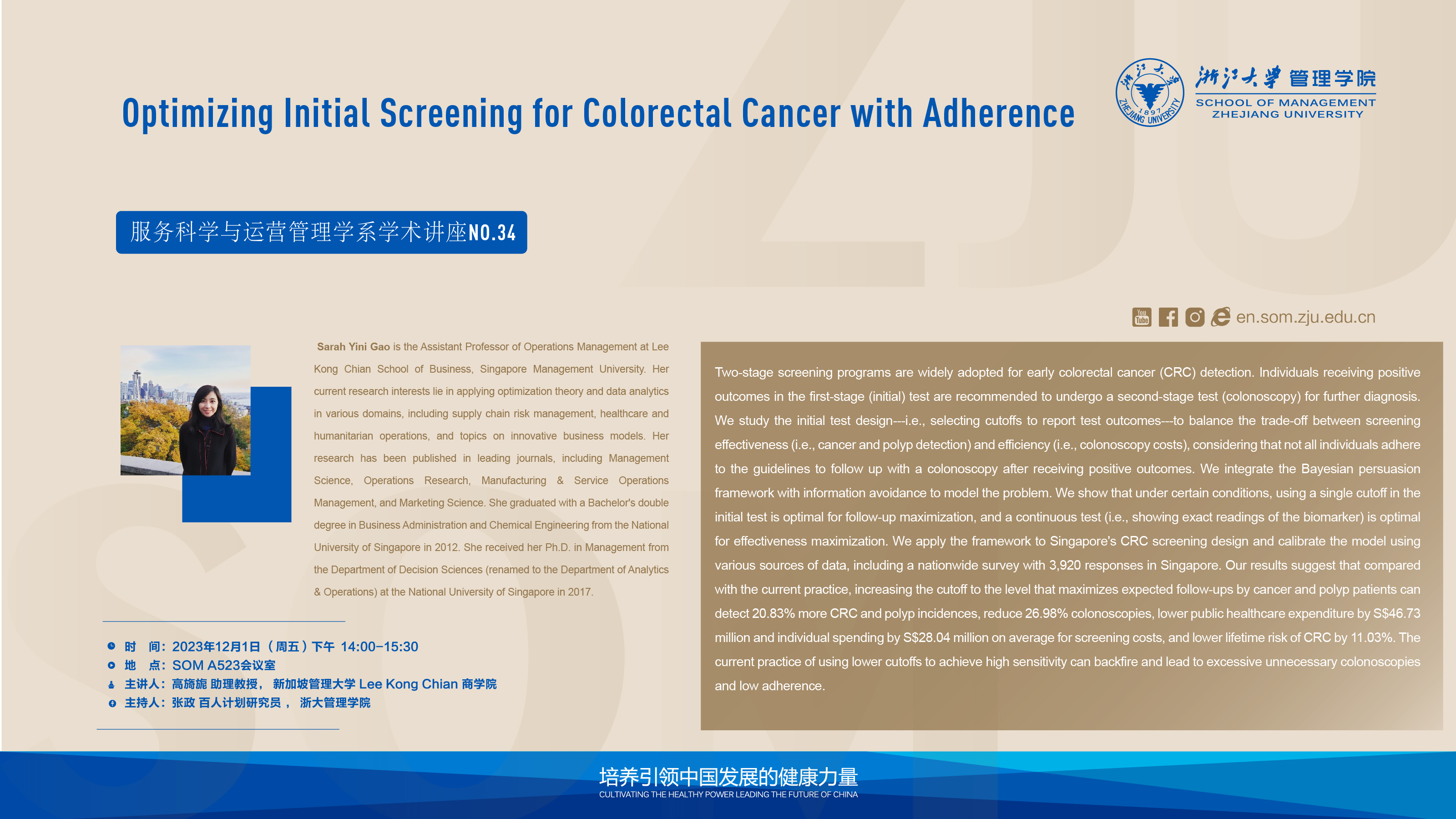
Workshop’s Topic: Two-stage screening programs for the early detection of colorectal cancer (CRC) are widespread. Individuals who test positive in the first test are recommended to undergo a second test (colonoscopy) for further diagnosis. We examine the design of the initial test, i.e. the selection of cut-off values for reporting test results, to find a trade-off between screening effectiveness (i.e. detection of cancer and polyps) and efficiency (i.e. the cost of colonoscopy), taking into account that not all individuals adhere to the guidelines and undergo colonoscopy after a positive result. We integrate the Bayesian belief framework with information avoidance to model the problem. We show that, under certain conditions, using a single cutoff value in the first test is optimal for maximizing follow-up and that a continuous test (i.e., the exact measure of the biomarker) is optimal for maximizing effectiveness. We apply the framework to the design of colorectal cancer screening in Singapore and calibrate the model using various data sources, including a nationwide survey with 3,920 responses in Singapore. Our results suggest that compared to current practice, increasing the cutoff to a level that maximizes expected follow-up screenings by cancer and polyp patents will detect 20.83% more colorectal cancer and polyp cases, reduce 26.98% colonoscopies, reduce public health expenditure by S$46.73 million and individual screening expenditure by S$28.04 million on average, and reduce lifetime risk of colorectal cancer by 11.03%. The current practice of using lower cut-offs to achieve high sensitivity may backfire and lead to excessive unnecessary colonoscopies and low adherence.
Time and Location: 14:00-15:30 PM (GMT+8), Room A523 (School of Management)
Language: Bilingual (Chinese and English)